1801006154 - LONG CASE 45 year old male with abdominal distension and pedal edema
1801006154
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment .
CASE:-
45 year old male complaints of abdominal distension and bilateral pedal edema (pitting type) , shortness of breath and scrotal swelling.
CHIEF COMPLAINTS:-
Patient complaints of
•Abdominal distension
•swelling over both legs
•Shortness of breath
•scrotal swelling
Since 25 days
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 6 years ago, then he had swellings over chest for which he went to hospital and was diagnosed as diabetic and was on medication since then.
•2 years ago when he went for routine checkup he was diagnosed as hypertensive and was on medication .
•6 months back patient's speech was reduced for which he went to a local hospital where he was found to have low GRBS (27 mg/dl) and he
also had jaundice and was advised to stop consuming alcohol.
•25days back he developed scrotal swelling, pedal edema, abdominal distension which was insidious in onset and gradually progressive, he also exhibited shortness of breath, for which he went to an RMP and was referred to KIMS, Narketpally.
• jaundice was present
• swelling of both legs was present.
PAST HISTORY:-
*History of Diabetes mellitus since 6 years and used tab.glibenclamide 5mg+ metformin 500mg, stopped taking medication since 6 months *History of hypertension since 2 years and taken Tab. Telma 40mg.
FAMILY HISTORY:- Insignificant.
PERSONAL HISTORY:-
•Diet:- mixed
•Appetite:- normal
•Sleep:- adequate 8 hrs per day
•Bowel and bladder :- regular
•Addictions:- ☆chronic alcoholic since 20years
-360 ml per day, stopped drinking since 1 month.
☆ Chronic smoker since 30 years - 2 packs per day .
•Occupational history:-hotel owner
GENERAL EXAMINATION:-
Patient is conscious, coherent and cooperative well oriented to time, place and person.
•Height:-158cm
•Abdominal girth: 124cm
VITALS:-
•Temperature: afebrile
•Pulse rate: 90bpm
•Respiratory rate: 22 cpm
•BP: 130/80 mmhg
•SpO2:98%
Pallor present, icterus present,Edema- bilateral pitting edema,cyanosis, clubbing, are absent .
SYSTEMIC EXAMINATION:-
●ABDOMINAL EXAMINATION:-
☆Inspection:
Abdominal distended
Flanks full
Umbilicus everted , and displaced downwards.
Engorged veins present
No visible peristalsis
No striae
No scars , sinuses .
☆Palpitation:
Superficial palpation:-no tenderness, no warmth, blood flow in veins is away from umbilicus.
Deep palpation:-
Soft non-tender
no hepatomegaly.
Splenomegaly present.
☆Percussion : Shifting dullness was present.Fluid thrill was present.
☆ Auscultation:- Bowel sounds heard, no venous hum and no splenic rub.
● CVS :- s1,s2, heard , no murmurs present.
●RESPIRATORY SYSTEM:- Normal vesicular breath sounds heard.
● CNS:- No focal neurological deficit seen.
INVESTIGATIONS:-
HEMOGRAM:-
Haemoglobin:- 10.4mg/dl
Total count :-6600cells/cumm
Neutrophils :-68%
Lymphocytes:-20%
Eosinophils :-2%
Monocytes :-10%
Basophils :-0%
Pcv :- 31.5 volume%
Mcv :-114.1fl
Mch :-37.7pg
Mchc :-33%
Rdw-cv :- 15.6%
Rdw-sd :-66.8fl
Rbc count :- 2.76 millions/cumm
Platelet count:- 2 lakhs/cumm.
SMEAR:-
Rbc :- anisocytosis, with normocytes, macrocytes, macroovalocytes seen
Wbc:- within normal limits
Platelets:-adequate in number and distribution
Hemoparasites:- no hemoparasites seen
Impression:- Dimorphic anemia
COMPLETE URINE EXAMINATION:-
Color :- pale yellow
Appearance:- clear
Reaction:-acidic
Specific gravity:- 1.010( 1.001-1.035)
Albumin:- positive(+)
Sugars:- nil
Bile salts :- nil
Bile pigments:- nil
Pus cells:- 4-5/ hpf
Epithelial cells:- 2-4/hpf
Rbc :- nil
Crystals:- nil
Casts:- nil
Amorphous deposits:-absent
Others:- nil
PROTHROMBIN TIME:-
prothrombin time:-20 sec(10-16 sec)
INR:- 1.4
APTT:-
Aptt test:- 39 sec( 24 -33 sec)
BLOOD UREA:-
Blood urea:-49 mg/dl (12-42mg/dl)
SERUM CREATININE:-
serum creatinine:- 1.2mg /dl(0.9-1.3mg/dl)
LIVER FUNCTION TESTS:-
Total bilirubin:- 4.78mg/dl(0-1mg /dl)
Direct bilirubin:- 2.91mg/dl(0-0.2mg/dl)
SGOT(AST):- 104 IU/L(0-35 IU/L)
SGPT(ALT):- 50 IU/L (0-45IU/L)
ALP :-260 IU/ L (53-128IU/L)
Total proteins:-7.7 gm/dl(6.4 -8.3 gm/dl)
Albumin:- 2.4 gm/dl(3.5 -5.2 mg/dl)
A/G ratio:- 0.46
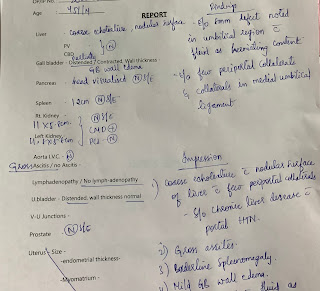
ULTRASONOGRAPHY ABDOMEN:-
ECG:-
Chest x ray:-
Hb:-9.4
Tlc:- 7100
Rbc:- 2.5
Platelets:- 1.7 lakh
Total bilirubin:-3.41
Direct bilirubin:-2.21
AST:-74
ALT:- 36
ALP:-218
Total proteins:- 6.7
Albumin:- 2.0
A/G:- 0.45
Sodium:-139
Potassium:-3.9
Chloride:-105
DAY 3:-
Hb:-8.9
Tc:-14,600
Pcv:- 26.8
Mcv:-110.5
Mch:-36.9
Mchc:-33.4
RBc:- 2.4
Platelets :- 1.7 lakhs
LFT:-
Total bilirubin:- 3.43
Direct bilirubin:- 2.09
AST:- 70
ALT:- 31
ALP:-208
Total proteins:- 6.3
Albumin:- 2.0
A/G :- 0.45
DAY 4:-
LFT:-
Total bilirubin:- 3.38
Direct bilirubin:-1.68
AST:-59
ALT:-30
ALP:-193
Total proteins:-6.4
Albumin:- 2.61
A/G:- 0.46
Creatinine:-1.0
Sodium:-140
Potassium:-4.1
Chloride:-99
Calcium:-0.98
PROVISIONAL DIAGNOSIS:-
Chronic liver disease with portal hypertension and ascites.
TREATMENT: -
1.Tab Lasix 80 mg po once daily
2.Tab Aldactone 50mg twice daily
3.Tab Lactulose 20ml once daily before going to bed.

















Comments
Post a Comment