32 year old male with complaints of yellowish discolouration of eye since 45 days.
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment .
32 year old gentleman who is a GHMC worker came to the hospital with chief complaints of
•yellowish discolouration of eyes since 45 days
•SOB since 10 days
• cough since 5 days
• fever since 3 days.
History of presenting illness:-
Patient was apparently asymptomatic 6 months back , then he developed yellowish discolouration of eyes .
• For this problem he used local medicine ( natuvedyam) and stopped consuming alcohol for about 3 months.
• Due to stopping of alcohol consumption his bilirubin levels came down , following which he again resumed consuming alcohol.
• After drinking alcohol ,he fought with his friend and injured his right arm causing fracture which was left untreated.( used natuvedyam).
• Recurrence of yellowish discolouration of eyes occurred after 1 month,again he started using natuvedyam .
•He also had an episode of GTCS 1 month ago after stopping alcohol for about 10 days.( alcohol withdrawal).
• Again yellowish discolouration occurred 1 month ago, then he stopped alcohol again.
•But this time , discolouration got progressed and his entire body turned yellow.
• C/o pedal edema, abdominal distension since 4 days.
•c/ o productive cough since 5 days.
•C/o SOB since 5 days which was grade 4.
•c/o fever since 3 days-low grade.
Past history:-
No history of DM, HTN, TB epilepsy, CAD.
Personal history :-
Diet- mixed
Appetite- normal
Sleep - adequate
Bowel and bladder movement- regular
Regularly consumes alcohol 90-180 ml of alcohol since 18 years.
General examination:-
he is conscious, coherent , cooperative, moderately built and moderately nourished.
Pallor - present.
Icterus -present.
Cyanosis- absent
Clubbing-absent.
Lymphadenopathy-absent.
Pedal edema -present.
Vitals:-
Temperature- 99°F
PR- 110bpm
Bp- 140/90 mmhg
RR- 20CPM
SPO2- 100%@ RA
GRBS -176 mg/dl.
Systemic examination:-
P/A:- soft, non tender, liver and spleen were palpable.
Bowel sounds -heard
Tremors - present.
CVS:- s1,s2 heard. No murmurs.
RS- BAE, NVBS heard.
CNS-no focal neurological deficit.
Provisional diagnosis:-
Acute or chronic liver disease
Hepatic encephalopathy-Grade 1 Hypokalemia.
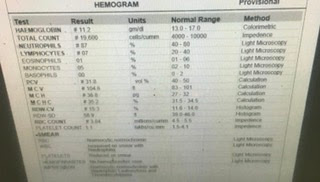
Investigations:-
Day 1 of admission:
Day 2 of admission:
Day 3 of admission:
Treatment:-
Inj.lasix 40mg iv/BD
Tab.aldactone 25mg PO/ BD
Temperature charting 4 holy
Tepid sponging SOS
Inj. Vit k 10 mg slow IV / OD
Syp. Ascoryl ls 10 ml PO/BD
Syp. Potchlor 10 ml in 1 glass of water PO/BD.
Syp.lactulose 10 ml P/O H/s
















.jpg)
Comments
Post a Comment