Hello and welcome to my blog!
(1) Self reflective writing on their medical student career
I'm Vishal Sarda, a passionate Intern and med student. Here,I share well organized, aesthetically,critically evaluated personal experience of my medical journey with enhanced patient interaction skills and overall patient approach in my med school.
I'd truly appreciate my HOD, professors, pg's for your time spent helping me in many occasions ,for challenging me to think critically and providing me with the tools.
I want to share some insights of information on particular treatments,medications and diseases.
Posted in General Medicine department from 1/12/2023 to 31/1/2024.
1/12/2023-31/12/2023= Unit postings.
1/1/2024- 15/1/2024= Psychiatry postings.
16/1/2024- 31/1/2024= Peripherals .
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
VISHAL SARDA
ROLL NO:-93
UNIT-I
This E blog also reflects my patient centered online learning portfolio .
(2) Evidence based data wise work flow blogs with verifiable links:-
UNIT POSTINGS:-
Blogs:-
Case-1:-
https://vishalsardarollno142.blogspot.com/2023/12/17-year-old-female-with-fever-since-1.html
Case-2:-
https://vishalsardarollno142.blogspot.com/2023/12/83-year-old-male-with-breathlessness.html
Case-3:-
https://vishalsardarollno142.blogspot.com/2023/12/75-year-old-female-with-nstemi-with.html
Case 4:-
https://vishalsardarollno142.blogspot.com/2023/12/45-year-old-female-with-pain-abdomen.html
Some of the other cases during my UG :-
Case-5:-
https://vishalsardarollno142.blogspot.com/2023/03/diabetic-ketoacidosis-with-perianal.html
Case-6:-
https://vishalsardarollno142.blogspot.com/2023/01/old-male-came-with-chief-complaints-of.html
Case-7:-
https://vishalsardarollno142.blogspot.com/2022/12/is-online-e-log-book-to-discuss-our.html
Case-8:-
https://vishalsardarollno142.blogspot.com/2022/11/18-year-old-boy-with-first-episode-of.html
Case-9:-
https://vishalsardarollno142.blogspot.com/2022/11/17-years-old-female-with-loose-stools.html
Case-10:-
https://vishalsardarollno142.blogspot.com/2022/10/45-year-old-male-with-abdominal.html
Case-11:-
https://vishalsardarollno142.blogspot.com/2021/12/32-year-old-male-with-complaints-of.html
Case-12:-
https://vishalsardarollno142.blogspot.com/2021/12/67-year-old-female-with-palpitations.html
Pajr:-
https://chat.whatsapp.com/De3ynQy6zD13EvOoIRlX7X
https://chat.whatsapp.com/FR7vWq7WSNkKPVBlicTsGS
Offline daily workflows-
CASES SEEN IN PSYCHIATRY:-
Cases seen in psychiatry:-
1.moderate depression with anxiety symptoms
2.OCD
3.Alcohol and tobacco dependence syndrome
4.Intellectual disability disorder
5.Adjustment disorder
6.schizophrenia
7.acute psychosis
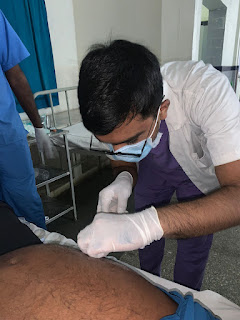
(3) Evidence of some of the procedures learnt and performed:-
Some procedures that I have performed during my posting in General Medicine and Peripherals:-
*Ascitic tap-
*2D-ECHO:-
Bedside OSCE discussion:-
*Abg samples taken -8
*Ryle's tube insertion.
*Blood samples, foley's catheterization.
*CPR done.
*During dialysis , monitored vitals and learnt about the procedure.
Central line(Internal jugular vein, femoral):-
Seen-12
During my nephrology postings, I got to see how chronic illness affects the patient and their families .
OSCE:-
Questions and reference links:-
(1)IRIDA- Iron refractory iron deficiency anaemia.
Iron refractory iron deficiency anemia is a hereditary recessive anemia due to a defect in the TMPRSS6 gene encoding Matriptase-2. This protein is a transmembrane serine protease that plays an essential role in down-regulating hepcidin, the key regulator of iron homeostasis. Hallmarks of this disease are microcytic hypochromic anemia, low transferrin saturation and normal/high serum hepcidin values.
It is mandatory to differentiate IRIDA from nutritional iron deficiency and from other genetic microcytic anemias. The presence of several affected siblings in the family may suggest the existence of an inherited disorder. However, many patients are sporadic cases because of the recessive mode of transmission and the small size of many pedigrees. In general, clinical data could help establish whether iron deficiency is inherited or acquired. Acquired iron deficiency may result from blood loss or decreased iron absorption, as in celiac disease, where anemia is the most common hematologic complication.Duodenal atrophy resulting in a delayed response to oral iron but a good response to intravenous iron is another confounding factor with IRIDA (see below: Iron therapy). A positive anti-endomysium antibody test, and a positive response to a gluten-free diet will rule out IRIDA.The age of onset may contribute to diagnosis since microcytic anemia is not present at birth in contrast to other genetic conditions such as DMT1 mutations or atransferrinemia. Sideroblastic anemia due to either ALAS-2 or SLC25A38 deficiency can also occur during childhood, but iron overload is also present in sideroblastic anemia as well as in DMT1 deficiency or atransferrinemia, as indicated by elevated serum iron and transferrin saturation. Microcytosis, hypochromia and low iron stores are present in both acquired iron deficiency and IRIDA. However, RBC count tends to be higher in IRIDA whereas in true iron deficiency serum ferritin is lower. Microcytosis and low mean corpuscular hemoglobin (MCH) are also hallmarks of beta-thalassemia carriers, who have normal or slightly elevated iron parameters and increased hemoglobin (Hb)A2.
(2)Ferritin and iron deficiency anaemia.
Ferritin is the best indicator of iron deficiency and a low ferritin alone is diagnostic of IDA. Iron is stored intracellularly as ferritin and in the presence of infection, malignancy or chronic inflammation, the ferritin rises as it is an acute phase protein. Therefore, the diagnosis of IDA is challenging when there is coexisting inflammation, as the ferritin can be up to 100 μg/L (normal range 20–200 μg/L in our institution), even in the presence of iron deficiency. In this case, further tests can help clarify the diagnosis.
(3)Candidiasis and iron deficiency anaemia:-
In order to obtain iron from the host, C. albicans may use either a high affinity reductive system, a siderophore uptake system or the hemoglobin–iron uptake system for iron acquisition (Moors et al., 1992; Ramanan and Wang, 2000; Lesuisse et al., 2002). Iron acquisition via the reductive system involves the reduction of ferric iron to the ferrous form with the subsequent transport of the reduced ferrous iron into the cell via a ferrous transporter complex (reviewed in Philpott, 2006). Although C. albicans has not been reported to use lactoferrin as an iron source, the reductive system can be used to acquire iron from sources such as ferritin and transferrin as well as free iron (Knight et al., 2005; Almeida et al., 2008). In C. albicans, two ferric reductases, Cfl1 (Fre1) (Yamada-Okabe et al., 1996; Hammacott et al., 2000) and Cfl95 (Fre10, Rbt2) (Knight et al., 2002), have been characterized. Within the C. albicans genome, there are as much as 17 ferric reductase-related genes but not all these genes are likely to be a ferric reductase. A functional ferric reductase has a ferric reductase domain and a FAD and/or NAD binding domain. These domains were absent in two of the reported reductases while another reductase was lacking a FAD and NAD binding domain (reviewed by Almeida et al., 2009). During iron acquisition, C. albicans ferric reductases Cfl1 and Cfl95, localized in the plasma membrane, reduce ferric iron to a soluble ferrous state (Xu et al., 2014b; Yu et al., 2014). Due to the spontaneous generation of toxic free radicals by ferrous iron, a multicopper oxidase enzyme is involved in the reconversion of the produced ferrous iron to a ferric state; a reaction known as ferroxidation (reviewed by Kosman, 2003; Almeida et al., 2009). The oxidation of iron by multicopper oxidases requires copper, and this is supplied by the intracellular copper transporter Ccc2 (Weissman et al., 2002). Finally, the iron permease, Ftr1, forms a complex with the multicopper oxidases to transport the ferric iron into the cell (Ziegler et al., 2011; Mamouei et al., 2017). Another mechanism of iron acquisition in C. albicans is via the low molecular weight ferrichrome as well as ferrioxamine-type siderophores which chelate iron with a high affinity (Minnick et al., 1991; Ardon et al., 2001). The analysis of the C. albicans genome has not revealed a siderophore synthesis pathway (Lan et al., 2004). In C. albicans, there is only one siderophore transporter which is the Sit1/Arn1 transporter. Since C. albicans does not directly produce siderophores, it then takes up xenosiderophores using the Sit1/Arn1 transporter or reductive iron uptake pathway (Ardon et al., 2001; Heymann et al., 2002).
The uptake of iron from haem proteins does not depend on the high affinity system, but rather relies on the common in several fungal extracellular membrane (CFEM) proteins (Kuznets et al., 2014). The CFEM domain is characterized by eight cysteine residues of conserved spacing and commonly found in many fungi membrane proteins (Kulkarni et al., 2003). In C. albicans, CFEM proteins namely Rbt5, Pga10 (Weissman and Kornitzer, 2004; Weissman et al., 2008), Pga7 (Kuznets et al., 2014), and Csa2 (Nasser et al., 2016) are responsible for haem iron uptake.
During infection, nutritional immunity, and iron-binding proteins may make iron largely unattainable, however, during commensalism in the oral cavity and gastrointestinal tract, iron may be more freely available. This forces a need on C. albicans to regulate iron acquisition to circumvent iron toxicity as well as iron deficiency in environments with different iron availability (Kronstad, 2013). The robustness of iron acquisition is tightly linked to the stage of infection, for example, in the initial stage of infection, gene expression is characterized by a strong iron acquisition strategy due to limited iron availability, whereas during the late infection stage, more iron is available due to extensive tissue damage
(4) Anaemia of chronic disease vs Iron deficiency anemia.
The major difference between ACD and IDA is that in IDA there is an absolute lack (serum ferritin below 30 ng/mL) [1] of iron, while the pathogenesis of ACD is multifactorial and the iron though available is not accessed by the young erythroid precursors.
In ACD, transferrin is increased while serum iron and transferrin saturation are reduced, while the erythrocyte-free protoporphyrin, serum ferritin, and marrow-stainable iron are increased . In ACD, the reduced transferrin saturation is not only due to lack of iron, but also due to increased production of transferrin. The hypoferraemia is due to trapping of iron in the cells of the reticulo-endothelial system, and the low serum iron consequently results in low transferrin saturation. The level of the transport protein transferrin is therefore increased in IDA but reduced or normal in ACD .
(5) Ultrasound measurement of bladder wall thickness in identifying bladder outlet obstruction.
Purpose: The objective of the study was to investigate specificity and sensitivity of bladder wall thickness in the diagnosis of bladder outlet obstruction.
Materials and methods: The study included 174 patients referred to our prostate centers for lower urinary tract symptoms. Free uroflowmetry and pressure-flow studies were performed in duplicate as part of the diagnostic evaluation. After the 2 voiding studies were done the bladder was filled to 150 ml. and wall thickness was measured via suprapubic ultrasound. Bladder outlet obstruction was diagnosed and graded according to the Abrams-Griffiths and Schäfer nomogram as well as to the group specific urethral resistance algorithm.
Results: A significant correlation (r > 0.6, p < or = 0.007) was found between bladder wall thickness and all parameters of the pressure-flow study. A bladder wall thickness of 5 mm. appeared to be the best cutoff point to diagnose bladder outlet obstruction, since 63.3% of patients with bladder wall thickness less than 5 mm. were unobstructed while 87.5% of those with a bladder wall thickness 5 mm. or greater were obstructed. Bladder wall thickness out performed uroflowmetry in terms of specificity and sensitivity in the diagnosis of outlet obstruction as demonstrated by an area under curve value of 0.860 versus 0.688 in the receiver operator characteristics analysis.
Conclusions: Measurement of bladder wall thickness appears to be a useful predictor of outlet obstruction with a diagnostic value exceeding free uroflowmetry although it does not represent a substitution to invasive urodynamics. These data support the hypothesis that the relationships between morphology and function are of clinical importance































.jpg)
Comments
Post a Comment